CareSource in Ohio provides healthcare coverage, but What Is The Income Limit For Caresource In Ohio to qualify? The income limit for CareSource in Ohio varies depending on the specific program and your family size; understanding these limits is crucial for accessing healthcare benefits and exploring partnership opportunities with income-partners.net, which can help you navigate eligibility requirements and discover pathways to increase your income. Understanding the income requirements for CareSource and other Medicaid programs allows you to strategically plan for your healthcare needs.
1. Understanding Ohio Medicaid Long-Term Care
Medicaid offers healthcare coverage to low-income individuals of all ages. This includes long-term care options for Ohio residents aged 65 and older. Ohio Medicaid offers coverage in nursing homes, assisted living facilities, and also supports seniors in their homes with non-medical services. Three main categories exist for long-term care programs:
- Institutional / Nursing Home Medicaid: This is an entitlement program, so all eligible individuals receive assistance, but benefits are limited to nursing home care.
- Medicaid Waivers / Home and Community Based Services (HCBS): This program isn’t an entitlement, meaning enrollment is limited, and waiting lists are possible. HCBS aims to prevent or delay nursing home admissions by offering services at home, in adult day care settings, or in assisted living facilities.
- Regular Medicaid / Aged, Blind, or Disabled (ABD): This is an entitlement program that provides various long-term care benefits, such as personal care assistance or adult day care.
While funding comes from both the state and federal governments, the Ohio Department of Medicaid (ODM) oversees the program within the established federal guidelines.
2. Navigating Income and Asset Limits for Ohio Medicaid Eligibility
Eligibility for Ohio Medicaid’s long-term care programs hinges on both financial and medical criteria, with income and asset limits varying across the different categories. These financial requirements are not static; they are subject to annual adjustments and fluctuate based on marital status. Ohio also offers alternative pathways to eligibility, which can further complicate the landscape. Let’s break down the basic financial requirements for single applicants in 2025 seeking Nursing Home Medicaid:
- Income Limit: Your monthly income must be under $2,901.
- Asset Limit: Your total assets must not exceed $2,000.
- Level of Care: You must demonstrate a need for a Nursing Home Level of Care.
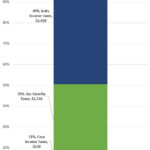
The following table provides a summary of the 2025 Ohio Medicaid Long-Term Care Eligibility criteria for seniors:
| 2025 Ohio Medicaid Long-Term Care Eligibility for Seniors |
|---|
| Type of Medicaid |
| Institutional / Nursing Home Medicaid |
| Medicaid Waivers / Home and Community Based Services |
| Regular Medicaid / Aged Blind and Disabled |
*All of a beneficiary’s monthly income, with the exception of a Personal Needs Allowance of $50 / month, Medicare premiums, and possibly a Needs Allowance for a non-applicant spouse (if applicable), must be paid to the nursing home. This is called a Patient Liability. †Based on one’s living setting, a program beneficiary may not be able keep monthly income up to this level.
Those eligible for SSI are automatically approved for Medicaid in Ohio.
3. Defining Countable vs. Non-Countable Income for Ohio Medicaid
When determining Medicaid eligibility, it’s essential to understand what income counts and what doesn’t. Here’s a breakdown:
- Countable Income: Almost all income received by a Medicaid applicant counts toward the income limit. This includes wages, alimony, pension payments, Social Security Disability Income, Social Security Income, IRA withdrawals, and stock dividends.
- Non-Countable Income: Some types of income are exempt. Nationally, Holocaust restitution payments are excluded. In Ohio, the Veteran’s Aid & Attendance benefit (above the Basic VA Pension) is also not counted.
4. How Ohio Medicaid Treats Income for Married Couples
The way income is handled for married couples depends on whether one or both spouses are applying for Medicaid. Let’s clarify the rules:
- One Spouse Applying for Nursing Home Medicaid or a Waiver: Only the applicant’s income is considered. The income of the non-applicant spouse is disregarded entirely. The non-applicant spouse (also called the community spouse) may also be entitled to a Minimum Monthly Maintenance Needs Allowance (MMMNA) from their applicant spouse. The MMMNA ensures the community spouse has enough income to avoid financial hardship.
- Ohio’s MMMNA: As of July 1, 2025, the MMMNA in Ohio is $2,643.75. If the community spouse’s income falls below this amount, income can be transferred from the applicant spouse to bring them up to this level.
- Increased Income Allowance: The community spouse can further increase their income allowance if their housing and utility costs exceed a “shelter standard,” which is $793.13 per month (as of July 1, 2025). However, a Spousal Income Allowance cannot push the non-applicant’s monthly income over $3,948, which is the Maximum Monthly Maintenance Needs Allowance for 2025.
- One Spouse Applying for Regular Medicaid: In this case, the income of both spouses is considered when determining the applicant’s eligibility. There is no Monthly Maintenance Needs Allowance for the non-applicant spouse in this scenario.
5. Understanding Asset Definitions and Exceptions for Ohio Medicaid
When applying for Medicaid in Ohio, it’s essential to know which assets are counted and which are exempt. Let’s break it down:
- Countable Assets: These are assets that Medicaid includes when determining eligibility. They include cash, stocks, bonds, investments, and bank accounts (checking, savings, and credit union). Real estate that is not your primary residence is also considered a countable asset.
- Non-Countable (Exempt) Assets: Medicaid doesn’t count these assets towards the eligibility limit. Exempt assets include personal belongings, household furnishings, an automobile, and irrevocable burial trusts. In Ohio, IRAs and 401(k)s in “payout status” (meaning you’re taking Required Minimum Distributions) are also exempt. Your primary home is generally exempt as well.
6. How Ohio Medicaid Treats Assets for Married Couples
When determining Medicaid eligibility for a married couple, Ohio considers all assets to be jointly owned, regardless of which spouse owns them and regardless of the specific long-term care Medicaid program applied for. However, there’s an important exception:
- Community Spouse Resource Allowance (CSRA): The non-applicant spouse of a Medicaid Nursing Home or Waiver applicant is entitled to a Community Spouse Resource Allowance (CSRA). This allowance allows the community spouse (the non-applicant) to retain a portion of the couple’s assets.
- 2025 CSRA Limits: In 2025, the community spouse can keep 50% of the couple’s assets, up to a maximum of $157,920. However, if 50% of the assets is less than $31,584, the community spouse can retain 100% of the couple’s assets, up to $31,584.
- No CSRA for Regular Medicaid: It’s important to note that the Community Spouse Resource Allowance does not apply to Regular Medicaid.
7. Navigating Ohio Medicaid’s Look-Back Period
Ohio, like many states, has a Medicaid Look-Back Period. Here’s what you need to know:
- What it is: The Look-Back Period is a 5-year period that Medicaid examines before the date you apply for Nursing Home Medicaid or a Medicaid Waiver.
- What Medicaid checks: During this period, Medicaid scrutinizes all asset transfers you’ve made. They want to ensure you haven’t given away assets or sold them for less than fair market value.
- Why they do it: The purpose is to prevent people from deliberately reducing their assets to become eligible for Medicaid. Medicaid assumes that if you transfer assets during this period, it was done to meet the asset limit.
- Penalties for Violating the Look-Back: If Medicaid determines you violated the Look-Back Rule, you’ll be penalized with a period of Medicaid ineligibility. The length of the ineligibility period depends on the value of the assets transferred.
- Important Note: The Look-Back Period does not apply to Regular Medicaid.
- IRS Gift Tax Exemption: The IRS allows you to gift up to $19,000 per recipient per year (in 2025) without having to file a Gift Tax Return. However, gifting under this exemption still violates Medicaid’s Look-Back Period.
According to research from the University of Texas at Austin’s McCombs School of Business, gifting assets can trigger Medicaid penalties due to the Look-Back Rule, even if the gifts are within the IRS annual gift tax exclusion.
8. Understanding Ohio Medicaid’s Home Exemption Rules
Your home is often one of your most valuable assets, so it’s essential to understand how Ohio Medicaid treats it. Here’s a breakdown of the home exemption rules:
- Occupancy Requirement: To be exempt, the Medicaid applicant or their spouse must live in the home.
- Home Equity Interest Limit: If there is no spouse living in the home, there’s a home equity interest limit of $730,000 in 2025. Home equity is the current market value of your home minus any outstanding debt (like a mortgage). Equity interest refers to the portion of the home’s equity that the applicant owns.
- Intent to Return: If neither the applicant nor their spouse lives in the home, the applicant must demonstrate an “Intent to Return” to the home. This means they must show they plan to return home at some point in the future.
- No Home Equity Interest Limit for Regular Medicaid: It’s important to note that there is no home equity interest limit for Regular Medicaid.
- Estate Recovery Program: While your home is generally exempt from Medicaid’s asset limit during your lifetime, it’s not exempt from Medicaid’s Estate Recovery Program.
Following a long-term care Medicaid beneficiary’s death, Ohio’s Medicaid agency may attempt to recover the costs of care they provided from the deceased’s estate. The home is often the most valuable asset in the estate, and without proper planning, it may be used to reimburse Medicaid instead of being passed on to family members as inheritance.
9. Meeting Medical and Functional Need Requirements for Ohio Medicaid
To qualify for long-term care Medicaid in Ohio, you must demonstrate a medical need for that level of care. Here’s how that works:
- Nursing Home Medicaid and Medicaid Waivers: These programs require a Nursing Facility Level of Care (NFLOC). This means your medical condition must be severe enough that you would require the level of care provided in a nursing home. Some program benefits may have additional requirements. For example, to receive home modifications, you might need to prove that you can’t safely live at home without those modifications.
- Regular Medicaid: For long-term care services through Regular Medicaid, you need to demonstrate a functional need with Activities of Daily Living (ADLs). This means you require assistance with everyday tasks like bathing, dressing, or eating. However, a Nursing Facility Level of Care is not necessarily required for Regular Medicaid.
10. Qualifying for Ohio Medicaid When Over the Income or Asset Limits
Even if you don’t meet the standard financial eligibility requirements for Ohio Medicaid, you may still be able to qualify. Here are some strategies:
- Qualified Income Trusts (QITs): Also known as Miller Trusts, QITs are a way for individuals whose income exceeds Medicaid’s limit to become income-eligible for Nursing Home Medicaid or a Medicaid Waiver.
- How they work: You deposit your “excess” income into the trust. For Medicaid purposes, the money in the QIT doesn’t count towards your income limit. The trust must be irrevocable, meaning its terms cannot be changed or canceled.
- Trustee: A trustee manages the trust and has legal control over the funds. The funds can only be used for very specific purposes, such as paying for medical expenses incurred by the Medicaid enrollee.
- Asset Spend Down: If your countable assets exceed Ohio Medicaid’s asset limit, you can “spend down” those assets on non-countable ones to become asset-eligible.
- Examples of acceptable spend-down: Home modifications (wheelchair ramps, stair lifts), prepaying funeral and burial expenses, and paying off debt.
- Important Reminder: You cannot gift assets or sell them for less than fair market value within 60 months of applying for Nursing Home Medicaid or a Medicaid Waiver. This would violate Medicaid’s Look-Back Rule and result in a penalty. Keep detailed records of how you spend down assets to prove you didn’t violate the rule.
- Medicaid Planning: Many individuals seeking Medicaid are over the income and/or asset limits but still can’t afford their cost of care. Medicaid planning can help.
- Medicaid Planning Professionals: By working with a Medicaid Planning Professional, families can employ various strategies to become Medicaid-eligible and protect their primary home from Medicaid’s Estate Recovery Program.
11. Exploring Specific Ohio Medicaid Programs for Long-Term Care
Ohio Medicaid offers several programs to help seniors live in their homes and communities, in addition to nursing home care.
- PASSPORT Waiver: This waiver, formally known as Pre-Admission Screening System Providing Options & Resources Today, allows Ohioans to receive various long-term services and supports. These may include adult day care, home care, home modifications, and medical equipment/supplies.
- Assisted Living Waiver: This waiver assists individuals aged 21 and over in living in residential care facilities and assisted living residences. While it doesn’t cover the cost of room and board, it does pay for care services. Not all assisted living residences in Ohio accept waiver participants, so it’s crucial to check.
- MyCare Ohio: This is a mandatory managed care Medicaid program available in 29 Ohio counties for individuals who are dually eligible for both Medicaid and Medicare. Benefits can include adult day care, assisted living services, memory care services, home modifications, meal delivery, personal emergency response systems, and more.
- Program of All-Inclusive Care for the Elderly (PACE): PACE combines the benefits of Medicaid (including long-term care) and Medicare into a single program. It may also offer additional benefits like dental and eye care.
- Money Follows the Person (MFP): In Ohio, this program is also known as HOME Choice. This federal initiative helps individuals in institutions who are eligible for Medicaid transition back home or into the community.
12. Applying for Ohio Medicaid: A Step-by-Step Guide
Applying for long-term care Medicaid in Ohio can be done in several ways:
- Online: Through the Ohio Benefits website.
- Phone: Via the Consumer Hotline at 1-800-324-8680.
- In Person: At your county’s Job and Family Services office.
Your local Area Agency on Aging can also provide valuable assistance by answering questions about Medicaid programs and offering application support. Keep in mind that the application process may vary depending on the specific program you’re applying for. Before applying, make sure you meet all eligibility requirements. If your income and/or assets exceed the limits, Medicaid planning is strongly recommended.
The application process can be complex, as you’ll need to include extensive documentation with your application. Familiarizing yourself with the general application process for long-term care Medicaid can be beneficial.
13. Maximizing Your Income Potential Through Strategic Partnerships
Now that you understand the income limits for CareSource and other Medicaid programs in Ohio, let’s explore how you can increase your income through strategic partnerships. Income-partners.net is a valuable resource for individuals looking to connect with potential business partners and expand their income opportunities.
By leveraging the platform, you can:
- Discover Diverse Partnership Types: Explore various partnership models, including strategic alliances, joint ventures, and referral partnerships, to find the best fit for your skills and goals.
- Build Trusting Relationships: Learn strategies for building strong, trust-based relationships with potential partners, ensuring long-term success and mutual benefit.
- Negotiate Mutually Beneficial Agreements: Access resources and guidance on negotiating partnership agreements that are fair, equitable, and aligned with your financial objectives.
- Manage and Maintain Partnerships: Gain insights into effective partnership management practices, including communication strategies, conflict resolution techniques, and performance evaluation methods.
- Identify New Opportunities: Stay informed about emerging partnership trends and opportunities in the market, allowing you to proactively seek out lucrative collaborations.
14. Addressing Common Challenges in Finding the Right Business Partner
Many individuals face challenges when seeking out business partnerships. These challenges include:
- Finding partners who share your vision and goals.
- Building trust and rapport with potential collaborators.
- Negotiating fair and equitable partnership agreements.
- Managing conflicts and disagreements effectively.
- Measuring the success of your partnerships.
Income-partners.net offers solutions to these challenges by providing:
- A platform for connecting with like-minded individuals.
- Resources for building strong and trusting relationships.
- Templates and guidance for creating comprehensive partnership agreements.
- Tools and strategies for managing conflicts and measuring partnership performance.
By addressing these challenges head-on, you can increase your chances of forming successful and profitable business partnerships.
15. Income-Partners.Net: Your Gateway to Lucrative Partnerships and Increased Income
Navigating the complexities of healthcare coverage and financial planning can be overwhelming, but income-partners.net is here to guide you. Our platform offers a wealth of resources and opportunities to help you increase your income and achieve your financial goals.
Here’s how income-partners.net can help you:
- Connect with Potential Partners: Our platform connects you with a diverse network of entrepreneurs, investors, and professionals seeking collaborative opportunities.
- Explore Partnership Strategies: Access a library of articles, guides, and templates on various partnership strategies, helping you find the best fit for your skills and goals.
- Build Strong Relationships: Learn proven techniques for building trust, communication, and rapport with potential partners, ensuring long-term success.
- Negotiate Mutually Beneficial Agreements: Our resources guide you through the process of negotiating partnership agreements that are fair, equitable, and aligned with your financial objectives.
- Stay Informed: Stay up-to-date on the latest partnership trends, opportunities, and best practices through our blog and newsletter.
By leveraging the power of strategic partnerships, you can unlock new income streams, expand your business reach, and achieve financial security.
FAQ: Understanding Income Limits for CareSource in Ohio
- What is CareSource?
CareSource is a managed care organization providing health insurance plans, including Medicaid, in Ohio. - What is the income limit to qualify for CareSource in Ohio?
The income limit varies depending on the specific CareSource plan and household size. Generally, it aligns with Ohio Medicaid income limits. - How do I find the exact income limit for my situation?
Visit the Ohio Medicaid website or contact CareSource directly to get the most accurate and up-to-date information. - What types of income are considered when determining eligibility?
Most income sources are considered, including wages, salaries, self-employment income, Social Security benefits, and retirement income. - Are there any income deductions allowed?
Certain deductions, such as childcare expenses and medical expenses, may be allowed. Check with CareSource or Ohio Medicaid for details. - What happens if my income exceeds the limit?
You may still qualify through spend-down programs or by exploring other Medicaid options with higher income limits. - Can assets affect my eligibility for CareSource?
Yes, some CareSource plans have asset limits. These limits vary, so it’s important to check the specific plan requirements. - How often are income limits updated?
Income limits are typically updated annually by Ohio Medicaid. - Where can I apply for CareSource in Ohio?
You can apply through the Ohio Benefits website or by contacting CareSource directly. - Does income-partners.net provide assistance with CareSource applications?
No, income-partners.net focuses on helping you increase your income through partnerships, which can indirectly improve your eligibility for various programs.
Ready to Explore Lucrative Partnership Opportunities?
Don’t let complex eligibility requirements hold you back from achieving your financial goals. Visit income-partners.net today to discover a world of strategic partnerships, innovative income-generating strategies, and expert resources to help you thrive!
Address: 1 University Station, Austin, TX 78712, United States
Phone: +1 (512) 471-3434
Website: income-partners.net