Does Medicaid Count Ssi As Income, potentially impacting your eligibility? At income-partners.net, we understand navigating the complexities of Medicaid eligibility can be daunting, especially when it comes to Social Security benefits. We’re here to provide clarity and solutions, focusing on how Supplemental Security Income (SSI) interacts with Medicaid’s income assessment. This article will explore the nuances of MAGI, Social Security benefits, and Medicaid eligibility. We will also help you understand earned income and unearned income.
1. Understanding Supplemental Security Income (SSI) and Medicaid Eligibility
Does Medicaid count SSI as income when determining eligibility? The simple answer is no, Supplemental Security Income (SSI) is generally not counted as income when determining eligibility for Medicaid. Let’s delve deeper into this crucial aspect of Medicaid eligibility and understand its implications.
SSI is a needs-based program designed to provide financial assistance to individuals with limited income and resources who are either aged, blind, or disabled. Medicaid, on the other hand, provides healthcare coverage to eligible individuals and families with low incomes. Since SSI is designed to support those with very limited means, it is typically excluded from the income calculation for Medicaid eligibility. This exclusion ensures that individuals receiving SSI can also access the healthcare benefits provided by Medicaid without losing their eligibility.
1.1 The Purpose of SSI Exclusion
The exclusion of SSI from Medicaid’s income calculation serves several important purposes:
- Ensuring Access to Healthcare: It guarantees that vulnerable populations, who rely on SSI for basic needs, can also access essential healthcare services through Medicaid.
- Preventing Double Counting: Counting SSI as income for Medicaid eligibility would effectively penalize individuals already identified as needing financial assistance.
- Simplifying the Application Process: Excluding SSI simplifies the eligibility determination process, making it easier for individuals and state agencies to administer these programs.
1.2 State Variations in Medicaid Eligibility
While the federal government sets the general guidelines for Medicaid, individual states have some flexibility in how they administer their programs. However, the exclusion of SSI from income calculations for Medicaid eligibility is a widely accepted practice across most states.
1.3 Other Types of Income and Medicaid Eligibility
It’s important to note that while SSI is excluded, other types of income can affect Medicaid eligibility. These may include:
- Social Security Retirement Benefits: These are often counted as income.
- Wages from Employment: Earnings from work can impact eligibility.
- Investment Income: Dividends, interest, and capital gains may be considered.
- Pension and Retirement Account Distributions: Income from these sources is generally counted.
1.4 Resources and Asset Limits
In addition to income, Medicaid also considers an applicant’s resources or assets. These may include bank accounts, stocks, bonds, and other valuable property. There are often limits on the amount of resources an individual can have and still qualify for Medicaid.
- Exempt Assets: Some assets, such as a primary residence and certain personal belongings, are typically exempt from consideration.
- Asset Limits: The specific asset limits vary by state and Medicaid program.
2. Modified Adjusted Gross Income (MAGI) and Medicaid
Does Medicaid count SSI as income under the MAGI system? Understanding the Modified Adjusted Gross Income (MAGI) is crucial for determining Medicaid eligibility. This section will define MAGI and explain which types of income are included and excluded.
MAGI is a method used to determine eligibility for Medicaid and premium tax credits for health insurance purchased through the Health Insurance Marketplace. It’s based on your adjusted gross income (AGI) with certain modifications.
2.1 Income Included in MAGI
The following types of income are typically included in MAGI:
- Wages, Salaries, and Tips: All taxable income from employment.
- Self-Employment Income: Income from running your own business.
- Unemployment Compensation: Benefits received while unemployed.
- Social Security Retirement, Disability, and Survivor Benefits: These are generally included unless specifically excluded.
- Pension and Retirement Income: Distributions from retirement accounts.
- Investment Income: Dividends, interest, and capital gains.
- Rental and Royalty Income: Income from property rentals and royalties.
- Alimony Received (for agreements finalized before 2019): Payments received as alimony.
2.2 Income Excluded from MAGI
Certain types of income are excluded from MAGI, including:
- Supplemental Security Income (SSI): As mentioned earlier, SSI is generally not included.
- Veterans’ Disability Benefits: Payments received for disabilities related to military service.
- Workers’ Compensation: Benefits received due to work-related injuries.
- Child Support Received: Payments received for the support of a child.
- Gifts: Money or property received as a gift.
- Loans: Funds received as loans (e.g., student loans, personal loans).
2.3 The Role of MAGI in Medicaid Eligibility
MAGI is used to determine if an individual or family meets the income requirements for Medicaid eligibility. States set specific income thresholds based on household size. If your MAGI is below the threshold for your state, you may be eligible for Medicaid.
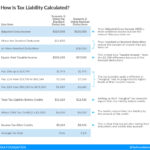
2.4 Example of MAGI Calculation
To illustrate how MAGI works, consider the following example:
- Wages: $30,000
- Social Security Retirement Benefits: $10,000
- Investment Income: $2,000
- Adjustments to Income (e.g., IRA contributions): $3,000
Calculation:
- Gross Income: $30,000 (Wages) + $10,000 (Social Security) + $2,000 (Investment Income) = $42,000
- Adjusted Gross Income (AGI): $42,000 (Gross Income) – $3,000 (Adjustments) = $39,000
- Modified Adjusted Gross Income (MAGI): In this case, since there are no other modifications, MAGI is the same as AGI, which is $39,000.
2.5 How MAGI Simplifies Eligibility Determination
MAGI was introduced as part of the Affordable Care Act (ACA) to simplify the eligibility determination process for Medicaid and premium tax credits. By using a standardized method based on tax return information, MAGI makes it easier for individuals to apply for coverage and for state agencies to verify income.
2.6 Changes in MAGI Rules
It’s important to stay informed about any changes to MAGI rules, as they can impact your eligibility for Medicaid. These rules can be updated by the federal government or by individual states. Consulting with a healthcare professional or visiting income-partners.net can provide the most up-to-date information.
3. Social Security Benefits and Medicaid Eligibility
Does Medicaid count SSI as income alongside other Social Security benefits? Let’s explore how different types of Social Security benefits are treated when determining Medicaid eligibility. Understanding the nuances of each benefit type is critical for accurate assessment.
The Social Security Administration (SSA) manages several benefits programs that provide financial assistance to individuals and their families. These programs include retirement benefits, disability benefits (SSDI and SSI), and survivor benefits.
3.1 Retirement Benefits
Social Security retirement benefits are paid to individuals who have worked and paid Social Security taxes for a certain number of years. The amount of the benefit is based on the individual’s earnings history.
- Treatment for Medicaid: Social Security retirement benefits are generally counted as income when determining Medicaid eligibility.
- Impact on Eligibility: Receiving Social Security retirement benefits can increase your MAGI, potentially affecting your eligibility for Medicaid.
3.2 Social Security Disability Insurance (SSDI)
Social Security Disability Insurance (SSDI) is paid to individuals who are unable to work due to a disability. To qualify for SSDI, you must have a sufficient work history and meet the SSA’s definition of disability.
- Treatment for Medicaid: SSDI benefits are also generally counted as income for Medicaid eligibility purposes.
- Coordination with Medicare: Individuals receiving SSDI may also be eligible for Medicare after a waiting period of two years.
3.3 Supplemental Security Income (SSI)
Supplemental Security Income (SSI) is a needs-based program that provides financial assistance to aged, blind, or disabled individuals with limited income and resources.
- Treatment for Medicaid: As previously mentioned, SSI benefits are typically excluded from income when determining Medicaid eligibility.
- Automatic Medicaid Eligibility: In many states, receiving SSI automatically qualifies you for Medicaid.
3.4 Survivor Benefits
Survivor benefits are paid to the surviving spouse and children of a deceased worker who had earned enough Social Security credits.
- Treatment for Medicaid: Survivor benefits are generally counted as income for Medicaid eligibility purposes.
- Exemptions for Children: There may be exemptions for children receiving survivor benefits if they do not meet the tax-filing thresholds for their earned and unearned income.
3.5 Dependent Benefits
Dependent benefits can be paid to the spouse and children of a Social Security beneficiary.
- Treatment for Medicaid: These benefits are also typically counted as income, although exemptions may exist for dependent children who do not meet tax-filing thresholds.
3.6 Concurrent Receipt of Benefits
In some cases, an individual may receive more than one type of Social Security benefit. For example, a person may receive both Social Security retirement benefits and SSDI.
- Impact on Medicaid: In these situations, all countable income, including both types of Social Security benefits, is considered when determining Medicaid eligibility.
3.7 State-Specific Rules
It’s important to be aware that Medicaid eligibility rules can vary by state. Some states may have different income thresholds or exemptions that could affect how Social Security benefits are treated.
3.8 Seeking Professional Guidance
Given the complexity of Social Security benefits and Medicaid eligibility, it’s often helpful to seek guidance from a qualified professional. A financial advisor or benefits counselor can provide personalized advice based on your specific circumstances. Visiting income-partners.net, you can find resources and professionals who can assist you.
4. Income Exemptions and Exclusions in Medicaid Eligibility
Does Medicaid count SSI as income despite some exemptions? Let’s discover the various income exemptions and exclusions that can impact Medicaid eligibility, ensuring you understand what income is protected. These exemptions can significantly affect an individual’s ability to qualify for Medicaid.
4.1 Standard Income Disregard
Many states offer a standard income disregard, which is a fixed amount that is subtracted from an individual’s gross income when determining Medicaid eligibility.
- Purpose: The standard income disregard helps to account for basic living expenses and can make more individuals eligible for Medicaid.
- Amount: The amount of the standard income disregard varies by state.
4.2 Earned Income Disregard
An earned income disregard allows individuals to exclude a portion of their earnings from employment when calculating their income for Medicaid eligibility.
- Purpose: This disregard incentivizes individuals to work and earn income without losing their Medicaid benefits.
- Example: Some states may allow individuals to exclude a certain percentage of their earned income, such as 50% or a fixed dollar amount.
4.3 Special Income Rules for Specific Populations
Certain populations, such as individuals receiving long-term care services or those with disabilities, may be eligible for special income rules that allow them to exclude additional income.
- Example: Individuals receiving long-term care in a nursing home may be able to exclude a portion of their income to pay for their care costs.
- Qualified Income Trusts (Miller Trusts): These trusts allow individuals with income above the Medicaid limit to become eligible by placing the excess income into the trust, which is then used to pay for medical expenses.
4.4 Exclusions for Certain Types of Income
In addition to SSI, there are other types of income that may be excluded from consideration when determining Medicaid eligibility.
- Examples: These may include certain types of educational grants, disaster relief assistance, and payments for foster care.
4.5 Income Averaging
Some states use a method called income averaging to calculate an individual’s income for Medicaid eligibility. This involves averaging income over a period of time, such as three or six months.
- Purpose: Income averaging can help to smooth out fluctuations in income and provide a more accurate picture of an individual’s financial situation.
4.6 Impact of Exemptions and Exclusions
Income exemptions and exclusions can significantly increase an individual’s chances of qualifying for Medicaid. By reducing the amount of countable income, these provisions make it easier to meet the income requirements for eligibility.
4.7 State-Specific Variations
It’s important to be aware that the specific income exemptions and exclusions available can vary by state. Some states may offer more generous provisions than others.
4.8 How to Claim Exemptions and Exclusions
To claim any applicable income exemptions or exclusions, individuals must typically provide documentation to the Medicaid agency. This may include pay stubs, tax returns, and other financial records.
5. Resources and Asset Limits for Medicaid Eligibility
Does Medicaid count SSI as income, and how do resources affect eligibility? Let’s examine the resource and asset limits that can impact Medicaid eligibility, ensuring you understand the constraints on your assets. Understanding these limits is essential for proper planning.
In addition to income, Medicaid also considers an applicant’s resources or assets when determining eligibility. These resources may include bank accounts, stocks, bonds, and other valuable property.
5.1 Resource Limits
Most Medicaid programs have limits on the amount of resources an individual can have and still qualify for benefits. These limits are typically quite low, often around $2,000 for an individual and $3,000 for a couple.
- Purpose: The resource limits are designed to ensure that Medicaid benefits are targeted to those with the greatest financial need.
5.2 Exempt Assets
Certain assets are typically exempt from consideration when determining Medicaid eligibility. These may include:
- Primary Residence: The home in which the individual lives is usually exempt, up to a certain equity value.
- Personal Belongings: Items such as clothing, furniture, and household goods are generally exempt.
- One Vehicle: One vehicle used for transportation is often exempt.
- Burial Funds: Funds set aside for burial expenses may be exempt, up to a certain amount.
- Irrevocable Burial Trusts: Trusts established for funeral expenses are typically exempt.
- Life Insurance Policies: Life insurance policies with a face value below a certain amount may be exempt.
5.3 Countable Assets
Assets that are not exempt are considered countable resources and are subject to the Medicaid resource limits. These may include:
- Bank Accounts: Checking and savings accounts are generally countable.
- Stocks and Bonds: Investments in stocks and bonds are countable.
- Retirement Accounts: Retirement accounts, such as IRAs and 401(k)s, may be countable, although some states may offer certain protections.
- Real Estate: Real estate other than the primary residence is countable.
5.4 Asset Transfers and Look-Back Period
Medicaid has rules regarding asset transfers to prevent individuals from giving away their assets to become eligible for benefits.
- Look-Back Period: Medicaid typically has a look-back period, which is a period of time (usually five years) prior to applying for Medicaid during which any asset transfers are reviewed.
- Penalty for Transfers: If an individual transfers assets for less than fair market value during the look-back period, they may be subject to a penalty, which could delay their eligibility for Medicaid.
5.5 Spousal Impoverishment Protections
When one spouse needs Medicaid to pay for long-term care services, special rules apply to protect the income and assets of the other spouse, known as the community spouse.
- Community Spouse Resource Allowance (CSRA): The community spouse is allowed to retain a certain amount of the couple’s combined assets, known as the CSRA.
- Minimum Monthly Maintenance Needs Allowance (MMMNA): The community spouse is also entitled to a minimum monthly income, known as the MMMNA, to ensure they have enough to live on.
5.6 Medicaid Planning
Given the complexity of Medicaid’s resource and asset rules, many individuals engage in Medicaid planning to protect their assets and ensure they can qualify for benefits when needed.
- Strategies: Medicaid planning strategies may involve transferring assets to trusts, purchasing exempt assets, or using other legal means to reduce countable resources.
5.7 State Variations
It’s important to be aware that Medicaid resource and asset rules can vary by state. Some states may have different limits or exemptions than others.
6. How to Apply for Medicaid
Does Medicaid count SSI as income during the application process? Let’s guide you through the Medicaid application process, including required documentation and tips for a successful application. A smooth application process can help you secure the benefits you need.
Applying for Medicaid can be a complex process, but understanding the steps involved can help you navigate it more effectively.
6.1 Determine Eligibility
Before applying for Medicaid, it’s important to determine if you are likely to be eligible based on income, resources, and other requirements.
- Income Limits: Check the income limits for Medicaid in your state.
- Resource Limits: Ensure that your resources are below the allowable limits.
- Other Requirements: Review any other eligibility requirements, such as residency and citizenship.
6.2 Gather Required Documentation
To apply for Medicaid, you will need to gather certain documentation to verify your eligibility. This may include:
- Proof of Identity: Driver’s license, passport, or other government-issued ID.
- Social Security Card: To verify your Social Security number.
- Proof of Income: Pay stubs, tax returns, Social Security statements, or other documents showing your income.
- Proof of Resources: Bank statements, investment statements, property deeds, or other documents showing your assets.
- Proof of Residency: Utility bills, lease agreements, or other documents showing your address.
- Medical Records: If applying for Medicaid based on disability, you may need to provide medical records to support your claim.
6.3 Complete the Application
You can obtain a Medicaid application from your state’s Medicaid agency or online. The application will ask for information about your income, resources, household, and other relevant details.
- Accuracy: Be sure to answer all questions accurately and completely.
- Assistance: If you need help completing the application, you can contact your local Medicaid office or a community organization for assistance.
6.4 Submit the Application
Once you have completed the application, you can submit it to your state’s Medicaid agency. You may be able to submit the application online, by mail, or in person.
6.5 Interview
After submitting the application, you may be required to attend an interview with a Medicaid caseworker. The interview is an opportunity for the caseworker to ask you questions about your application and verify your eligibility.
- Preparation: Be prepared to answer questions about your income, resources, and other relevant information.
- Honesty: Answer all questions honestly and accurately.
6.6 Approval or Denial
After reviewing your application and conducting the interview, the Medicaid agency will make a decision about your eligibility. If you are approved, you will receive a Medicaid card and information about your benefits. If you are denied, you will receive a notice explaining the reasons for the denial and your right to appeal.
6.7 Appeal Process
If you are denied Medicaid benefits, you have the right to appeal the decision. The appeal process typically involves submitting a written request for a hearing.
- Deadline: Be sure to file your appeal within the specified deadline.
- Representation: You may be able to have an attorney or other representative assist you with your appeal.
6.8 Ongoing Responsibilities
Once you are approved for Medicaid, you have certain ongoing responsibilities, such as reporting any changes in your income, resources, or household.
- Timely Reporting: Report any changes promptly to avoid any disruption in your benefits.
- Renewal: You will also need to renew your Medicaid coverage periodically to ensure that you continue to be eligible.
6.9 Seeking Help
Navigating the Medicaid application process can be challenging. If you need assistance, consider contacting:
- Medicaid Agency: Your state’s Medicaid agency can provide information and assistance with the application process.
- Community Organizations: Many community organizations offer free or low-cost assistance to individuals applying for Medicaid.
- Legal Aid: Legal aid organizations may be able to provide legal assistance to individuals who have been denied Medicaid benefits.
7. State-Specific Medicaid Rules and Regulations
Does Medicaid count SSI as income differently across states? Let’s explore the variations in Medicaid rules and regulations across different states, ensuring you’re aware of your local guidelines. Understanding state-specific rules is crucial for accurate eligibility assessment.
Medicaid is a joint federal and state program, which means that while the federal government sets the general guidelines, individual states have some flexibility in how they administer their programs. This can lead to variations in Medicaid rules and regulations across different states.
7.1 Income Limits
Income limits for Medicaid eligibility can vary by state. Some states may have higher income limits than others, making it easier for individuals to qualify for benefits.
7.2 Resource Limits
Resource limits can also vary by state. Some states may have higher resource limits or more generous exemptions than others.
7.3 Medicaid Expansion
The Affordable Care Act (ACA) allowed states to expand their Medicaid programs to cover more low-income adults. States that have expanded Medicaid typically have higher income limits and broader eligibility criteria than states that have not expanded.
7.4 Covered Services
The services covered by Medicaid can vary by state. Some states may offer a more comprehensive package of benefits than others.
7.5 Managed Care
Many states use managed care organizations (MCOs) to deliver Medicaid services. Under a managed care system, Medicaid beneficiaries enroll in a private health plan that contracts with the state to provide covered services.
7.6 Waivers
States can apply for waivers from the federal government to implement innovative Medicaid programs that differ from the standard rules. These waivers can allow states to offer new services, target specific populations, or modify eligibility criteria.
7.7 Long-Term Care
Medicaid is a major payer of long-term care services, such as nursing home care and home-based care. The rules for Medicaid eligibility for long-term care can be particularly complex, with strict income and asset limits.
7.8 Estate Recovery
Some states have estate recovery programs, which allow them to recover the cost of Medicaid services from the estates of deceased beneficiaries.
7.9 State Websites
Each state has its own Medicaid agency website that provides detailed information about the state’s Medicaid program, including eligibility requirements, covered services, and application procedures.
7.10 Seeking Local Expertise
Given the variations in Medicaid rules and regulations across states, it’s often helpful to seek local expertise. A Medicaid expert or benefits counselor in your state can provide personalized advice based on your specific circumstances.
8. Common Misconceptions About Medicaid and SSI
Does Medicaid count SSI as income due to common misconceptions? Let’s clarify common misconceptions about Medicaid and SSI to help you avoid misunderstandings and make informed decisions. Addressing these misconceptions is essential for accurate planning and application.
There are several common misconceptions about Medicaid and SSI that can lead to confusion and inaccurate information.
8.1 Misconception 1: SSI Recipients Are Automatically Eligible for All Medicaid Services
While SSI recipients are often automatically eligible for Medicaid in many states, this is not always the case. Some states may require SSI recipients to meet additional eligibility requirements to receive certain Medicaid services.
8.2 Misconception 2: All Social Security Benefits Are Counted as Income for Medicaid
While most Social Security benefits are counted as income for Medicaid, SSI is generally excluded. It’s important to understand the specific rules for each type of Social Security benefit.
8.3 Misconception 3: Medicaid Is Only for the Very Poor
While Medicaid is designed to provide healthcare coverage to low-income individuals and families, the income limits for eligibility can vary by state. Some individuals with modest incomes may still be eligible for Medicaid.
8.4 Misconception 4: Medicaid Will Take Your Home
Medicaid has rules regarding asset transfers and estate recovery, but it is not likely to take your home if you meet certain conditions. The primary residence is often exempt from consideration for Medicaid eligibility, and there are protections in place for the community spouse when one spouse needs Medicaid to pay for long-term care services.
8.5 Misconception 5: You Can’t Have Any Assets to Qualify for Medicaid
While Medicaid has resource limits, there are certain assets that are exempt from consideration, such as a primary residence, personal belongings, and one vehicle.
8.6 Misconception 6: Applying for Medicaid Is Too Complicated
While the Medicaid application process can be complex, there are resources available to help you navigate it. Your state’s Medicaid agency, community organizations, and legal aid organizations can provide assistance with the application process.
8.7 Misconception 7: Medicaid Is the Same as Medicare
Medicaid and Medicare are two different government programs that provide healthcare coverage. Medicare is primarily for individuals age 65 and older or those with certain disabilities, while Medicaid is primarily for low-income individuals and families.
8.8 Misconception 8: You Can’t Work and Still Receive Medicaid
Some states offer earned income disregards that allow individuals to exclude a portion of their earnings from employment when calculating their income for Medicaid eligibility. This can make it possible to work and still receive Medicaid benefits.
9. Planning Strategies for Medicaid Eligibility
Does Medicaid count SSI as income, and how can you plan for eligibility? Let’s discuss effective planning strategies to help you meet Medicaid eligibility requirements while protecting your assets. Smart planning can make a significant difference in securing your eligibility.
Given the complexity of Medicaid’s income and resource rules, it’s often helpful to engage in Medicaid planning to protect your assets and ensure you can qualify for benefits when needed.
9.1 Understand the Rules
The first step in Medicaid planning is to understand the specific rules and regulations in your state. This includes income limits, resource limits, asset transfer rules, and estate recovery provisions.
9.2 Maximize Exempt Assets
One strategy is to maximize your exempt assets, such as your primary residence, personal belongings, and one vehicle. These assets are not counted when determining Medicaid eligibility.
9.3 Spend Down Strategies
If your countable assets exceed the Medicaid resource limits, you may need to “spend down” your assets to become eligible. This involves using your excess assets to pay for allowable expenses, such as medical bills, home improvements, or other necessary expenses.
9.4 Irrevocable Burial Trusts
You can establish an irrevocable burial trust to set aside funds for your funeral expenses. These trusts are typically exempt from Medicaid’s resource limits.
9.5 Qualified Income Trusts (Miller Trusts)
If your income exceeds the Medicaid income limits, you may be able to establish a qualified income trust (QIT), also known as a Miller Trust. This type of trust allows you to deposit your excess income into the trust, which is then used to pay for your medical expenses. The income deposited into the trust is not counted when determining Medicaid eligibility.
9.6 Transfer Assets
Transferring assets to a spouse, child, or other family member can be a way to protect your assets from Medicaid. However, it’s important to be aware of Medicaid’s asset transfer rules and the potential penalties for transferring assets for less than fair market value during the look-back period.
9.7 Long-Term Care Insurance
Purchasing long-term care insurance can help to cover the cost of long-term care services, reducing the need to rely on Medicaid.
9.8 Seek Professional Advice
Medicaid planning can be complex, so it’s often helpful to seek advice from a qualified attorney, financial advisor, or Medicaid planner. These professionals can help you develop a personalized plan that meets your specific needs and circumstances.
9.9 Charitable Giving
Consider making charitable donations to reduce your countable assets.
9.10 Home Improvements
Invest in necessary home repairs or modifications to improve safety and accessibility.
10. Resources for Further Information and Assistance
Does Medicaid count SSI as income, and where can you find more information? Let’s provide a list of valuable resources for obtaining further information and assistance with Medicaid and SSI-related matters. Access to reliable resources can empower you to make informed decisions.
There are many resources available to help you learn more about Medicaid and SSI and to assist you with the application process.
10.1 Social Security Administration (SSA)
The SSA is the government agency responsible for administering the SSI program. The SSA website provides information about SSI eligibility requirements, benefits, and application procedures.
10.2 Medicaid Agency
Your state’s Medicaid agency can provide information about Medicaid eligibility requirements, covered services, and application procedures.
10.3 Centers for Medicare & Medicaid Services (CMS)
CMS is the federal agency that oversees the Medicaid and Medicare programs. The CMS website provides information about Medicaid policies and regulations.
10.4 Legal Aid Organizations
Legal aid organizations provide free or low-cost legal assistance to low-income individuals. They can help you with Medicaid applications, appeals, and other legal issues.
10.5 Community Organizations
Many community organizations offer assistance to individuals applying for Medicaid and SSI. These organizations can provide information, counseling, and application assistance.
10.6 National Council on Aging (NCOA)
NCOA is a nonprofit organization that provides resources and support to older adults. The NCOA website provides information about Medicaid, Medicare, and other benefits programs.
10.7 AARP
AARP is a membership organization for people age 50 and older. The AARP website provides information about Medicaid, Medicare, and other issues of interest to older adults.
10.8 National Disability Rights Network (NDRN)
NDRN is a nonprofit organization that provides legal advocacy services to people with disabilities. The NDRN website provides information about Medicaid and other disability-related issues.
10.9 Area Agencies on Aging (AAA)
AAAs are local agencies that provide services and support to older adults. Your local AAA can provide information about Medicaid and other benefits programs.
10.10 Income-Partners.net
Income-partners.net offers valuable resources, strategies, and potential partnerships to help individuals increase their income and navigate complex financial systems like Medicaid.
10.11 State Health Insurance Assistance Programs (SHIPs)
SHIPs offer free counseling to Medicare beneficiaries and their families. They can provide information about Medicaid and Medicare and help you navigate the application process.
Navigating the complexities of Medicaid and SSI requires a clear understanding of eligibility rules, income and resource limits, and state-specific regulations. At income-partners.net, we aim to provide you with the knowledge and resources necessary to make informed decisions and secure the benefits you deserve. Remember, SSI is generally not counted as income for Medicaid eligibility, but other Social Security benefits and assets may affect your eligibility. By understanding these nuances and seeking professional guidance when needed, you can effectively plan for your healthcare needs and financial well-being.
Ready to explore partnership opportunities that can help you increase your income and navigate financial challenges? Visit income-partners.net today to discover strategies for building successful partnerships and achieving your financial goals.
FAQ: Medicaid and SSI
Here are some frequently asked questions (FAQ) about Medicaid and SSI.
- Does Medicaid count SSI as income?
No, Supplemental Security Income (SSI) is generally not counted as income when determining eligibility for Medicaid. - What is MAGI, and how does it affect Medicaid eligibility?
Modified Adjusted Gross Income (MAGI) is a method used to determine eligibility for Medicaid. It includes most taxable income, but excludes SSI, veterans’ disability benefits, and other specific income types. - Are Social Security retirement benefits counted as income for Medicaid?
Yes, Social Security retirement benefits are generally counted as income when determining Medicaid eligibility. - What assets are exempt from Medicaid’s resource limits?
Exempt assets typically include a primary residence, personal belongings, one vehicle, and certain burial funds. - What is the look-back period for Medicaid asset transfers?
Medicaid typically has a look-back period of five years, during which any asset transfers are reviewed for potential penalties. - What is a Qualified Income Trust (QIT), and how can it help with Medicaid eligibility?
A Qualified Income Trust (QIT), or Miller Trust, allows individuals with income above the Medicaid limit to become eligible by placing the excess income into the trust, which is then used to pay for medical expenses. - Can I work and still receive Medicaid benefits?
Some states offer earned income disregards that allow individuals to exclude a portion of their earnings from employment when calculating their income for Medicaid eligibility. - How do I apply for Medicaid?
You can apply for Medicaid through your state’s Medicaid agency. The application process typically involves providing documentation of income, resources, and other relevant information. - What happens if I am denied Medicaid benefits?
If you are denied Medicaid benefits, you have the right to appeal the decision. The appeal process typically involves submitting a written request for a hearing. - Where can I find more information about Medicaid and SSI?
You can find more information about Medicaid and SSI from the Social Security Administration (SSA), your state’s Medicaid agency, and community organizations. Also, visit income-partners.net for additional resources and assistance.