Is Medicaid Income Based? Yes, Medicaid eligibility is primarily income-based, but understanding the specifics can be complex. Income-partners.net simplifies this process, offering resources to navigate Medicaid requirements and explore partnership opportunities for increased financial stability. This article helps to understand Medicaid eligibility criteria, explore income-based qualifications, and identify strategies to leverage partnerships for financial well-being.
1. What Is Medicaid and How Does Income Affect Eligibility?
Medicaid provides health coverage to millions of Americans, and income plays a significant role in determining who qualifies.
Medicaid, together with the Children’s Health Insurance Program (CHIP), offers healthcare coverage to over 77.9 million Americans, encompassing children, pregnant women, parents, seniors, and individuals with disabilities. It stands as the largest single source of health coverage in the United States. While federal law mandates states to cover specific groups, such as low-income families and individuals receiving Supplemental Security Income (SSI), states can also choose to cover additional groups. The Affordable Care Act of 2010 further expanded Medicaid eligibility to include nearly all low-income Americans under 65. Generally, eligibility is determined by Modified Adjusted Gross Income (MAGI), but specific income limits vary by state and household size. Understanding these income thresholds is crucial for accessing Medicaid benefits.
According to the Centers for Medicare & Medicaid Services (CMS), Medicaid eligibility is largely determined by income, but other factors such as age, disability status, and family size also play a role. The income limits are set by each state, but they generally align with the Federal Poverty Level (FPL).
Income-partners.net can guide you through these intricacies and help you find ways to potentially increase your income through strategic partnerships, which may impact your Medicaid eligibility.
1.1 How Does Modified Adjusted Gross Income (MAGI) Impact Medicaid Eligibility?
MAGI is the primary method for determining income eligibility for most Medicaid applicants.
The Affordable Care Act (ACA) introduced MAGI as the standard for determining income eligibility for Medicaid, CHIP, and premium tax credits in the health insurance marketplace. MAGI considers taxable income and tax filing relationships to assess financial eligibility. This standardized approach simplifies the application process, ensuring individuals are directed to the appropriate program. Unlike the previous system, MAGI does not allow for income disregards or asset tests. This change streamlines the eligibility process, making it easier for individuals to apply and enroll in Medicaid.
MAGI includes:
- Adjusted Gross Income (AGI)
- Tax-exempt interest income
- Foreign earned income and housing expenses
MAGI simplifies the eligibility process by using a consistent set of income counting rules. This helps in accurately determining who qualifies for Medicaid based on their financial situation. However, some individuals, such as those eligible due to blindness, disability, or age (65 and older), are exempt from MAGI-based income counting rules.
1.2 What Are the Income Limits for Medicaid?
Income limits for Medicaid vary by state and household size, often tied to the Federal Poverty Level (FPL).
Each state sets its own income limits for Medicaid eligibility, generally based on a percentage of the Federal Poverty Level (FPL). For example, many states extend Medicaid coverage to adults with incomes at or below 133% of the FPL. These limits are adjusted annually, so it’s essential to check the current guidelines for your specific state. Factors such as household size also influence these limits, with higher income thresholds for larger families. Understanding these state-specific income limits is crucial for determining Medicaid eligibility.
To find the specific income limits for your state, you can visit the Medicaid website or contact your local Medicaid office. These resources provide detailed information on the current income thresholds and eligibility requirements.
- Example: In some states, a single adult may qualify with an income up to 138% of the FPL, while a family of four may qualify with a higher income threshold.
1.3 What Happens if My Income Exceeds the Medicaid Limit?
Even if your income exceeds the standard Medicaid limit, there are still pathways to eligibility.
If your income surpasses the standard Medicaid limit, you might still qualify through options like the Medically Needy program or a spend-down program. The Medically Needy program allows individuals with significant health needs to become eligible by “spending down” their income on medical expenses. By incurring expenses for medical care, individuals can reduce their countable income below the state’s medically needy income standard. Additionally, some states offer spend-down programs, enabling individuals to deduct medical expenses from their income to meet Medicaid eligibility requirements. These programs provide a crucial safety net for those with high medical costs.
Alternatives if your income is too high:
- Medically Needy Program: Allows individuals with high medical expenses to qualify.
- Spend-Down Program: Deduct medical expenses from income to meet eligibility.
- Partnerships: Explore partnership opportunities to manage income fluctuations and maintain eligibility, as suggested by income-partners.net.
1.4 What Non-Financial Factors Influence Medicaid Eligibility?
Besides income, Medicaid eligibility also depends on residency, citizenship, and specific group criteria.
Medicaid eligibility is not solely based on income; non-financial factors also play a significant role. Applicants must be residents of the state in which they are applying and must be either U.S. citizens or qualified non-citizens. Specific eligibility groups may have additional criteria, such as age, pregnancy status, or parenting status. For instance, some programs are limited to children or pregnant women. Meeting these non-financial requirements is essential for Medicaid approval, regardless of income level.
Non-financial requirements include:
- Residency in the state where applying.
- U.S. citizenship or qualified non-citizen status.
- Meeting specific criteria based on age, pregnancy, or parenting status.
2. Exploring Medicaid Eligibility Based on Specific Circumstances
Specific groups have tailored eligibility criteria, making it important to understand these nuances.
Medicaid eligibility varies significantly based on individual circumstances, such as age, family status, and disability. Children, pregnant women, and individuals with disabilities often have different income thresholds and eligibility criteria compared to other groups. Understanding these specific requirements is crucial for accessing the appropriate Medicaid benefits.
2.1 How Does Medicaid Eligibility Differ for Children and Pregnant Women?
Children and pregnant women often have more lenient income requirements for Medicaid eligibility.
Medicaid eligibility for children and pregnant women typically involves more lenient income requirements compared to other groups. Many states extend coverage to children with family incomes significantly above the federal poverty level (FPL). For pregnant women, Medicaid provides essential prenatal care and coverage throughout the pregnancy and postpartum period, often with higher income thresholds. These provisions ensure that vulnerable populations receive the necessary healthcare support.
Specifics include:
- Higher income thresholds for children and pregnant women.
- Coverage for prenatal care and postpartum services.
- Ensuring healthcare access for vulnerable populations.
2.2 What Are the Medicaid Rules for Seniors and Individuals With Disabilities?
Seniors and individuals with disabilities often have different eligibility criteria, including asset tests.
Medicaid eligibility for seniors and individuals with disabilities often involves different criteria than those based on MAGI. Eligibility may be determined using the income methodologies of the Supplemental Security Income (SSI) program, which includes both income and asset tests. Some states, known as 209(b) states, use more restrictive eligibility criteria than SSI but still largely apply SSI methodologies. These rules take into account the unique financial circumstances of seniors and individuals with disabilities, ensuring they can access necessary healthcare services.
Key considerations:
- Use of SSI income methodologies, including asset tests.
- Variations in eligibility criteria among states.
- Ensuring access to healthcare for vulnerable seniors and disabled individuals.
2.3 What Is the Role of the Affordable Care Act (ACA) in Expanding Medicaid?
The ACA significantly expanded Medicaid eligibility, particularly for low-income adults.
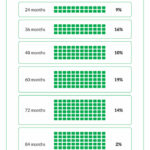
The Affordable Care Act (ACA) played a pivotal role in expanding Medicaid eligibility across the United States. It created the opportunity for states to extend Medicaid coverage to nearly all low-income Americans under age 65, with incomes at or below 133% of the federal poverty level (FPL). While most states have chosen to expand coverage to adults, those that have not yet expanded may do so at any time. This expansion has significantly increased access to healthcare for millions of Americans, particularly those who were previously uninsured.
ACA expansion impact:
- Expanded coverage to low-income adults under 65.
- Increased access to healthcare for millions of Americans.
- State-level decisions on whether to adopt the expansion.
2.4 How Do Waivers and Demonstrations Affect Medicaid Coverage?
States can use waivers to expand Medicaid coverage beyond traditional eligibility groups.
States can apply to the Centers for Medicare & Medicaid Services (CMS) for waivers and demonstrations to expand Medicaid coverage beyond traditional eligibility groups. These waivers allow states to implement innovative approaches to healthcare delivery and coverage. For example, states may use waivers to provide Medicaid to populations not traditionally covered under the state plan or to offer additional services. These waivers enable states to tailor their Medicaid programs to meet specific local needs and priorities.
Waiver benefits:
- Allows states to expand coverage to new populations.
- Enables innovative approaches to healthcare delivery.
- Tailors Medicaid programs to meet local needs.
3. Navigating the Medicaid Application Process
Understanding the application process can help ensure a smooth experience.
Applying for Medicaid can be a complex process, but understanding the steps involved can help ensure a smooth experience. Generally, the application process involves gathering necessary documentation, completing the application form, and submitting it to your local Medicaid office. Knowing what to expect and how to prepare can significantly increase your chances of a successful application.
3.1 What Documents Do I Need to Apply for Medicaid?
Gathering the right documents is crucial for a successful Medicaid application.
When applying for Medicaid, it’s essential to gather all necessary documentation to support your application. Common documents required include proof of income (such as pay stubs or tax returns), proof of residency (like a utility bill or lease agreement), and proof of citizenship or immigration status. Additionally, you may need to provide information about your household members and any existing health insurance coverage. Having these documents readily available can expedite the application process and prevent delays.
Required documents typically include:
- Proof of income (pay stubs, tax returns).
- Proof of residency (utility bill, lease agreement).
- Proof of citizenship or immigration status.
- Information about household members and existing health insurance.
3.2 How Do I Complete the Medicaid Application Form?
Accurately completing the application form is essential for Medicaid approval.
Completing the Medicaid application form accurately is crucial for ensuring your application is processed smoothly. Be sure to fill out all sections completely and provide accurate information. If you’re unsure about any questions, seek assistance from your local Medicaid office or a healthcare navigator. Review the form carefully before submitting it to avoid errors or omissions that could delay or deny your application.
Tips for completing the form:
- Fill out all sections completely and accurately.
- Seek assistance from Medicaid office or a healthcare navigator if needed.
- Review the form carefully before submitting.
3.3 What Happens After I Submit My Medicaid Application?
Knowing what to expect after submitting your application can reduce anxiety and ensure you stay informed.
After submitting your Medicaid application, the Medicaid agency will review your information to determine your eligibility. This process may involve verifying your income, residency, and other relevant factors. You may be contacted for additional information or documentation if needed. Once a decision is made, you will receive a notification regarding your eligibility status and, if approved, information about your Medicaid coverage.
Post-application steps:
- Medicaid agency reviews your information.
- Verification of income, residency, and other factors.
- Notification of eligibility status and coverage details.
3.4 What Are My Rights if My Medicaid Application Is Denied?
Understanding your appeal rights is important if your Medicaid application is denied.
If your Medicaid application is denied, you have the right to appeal the decision. The appeal process typically involves requesting a fair hearing, where you can present evidence and arguments to support your case. You will be notified of the reasons for the denial and provided with instructions on how to file an appeal. Understanding your appeal rights is crucial for ensuring you have the opportunity to challenge an unfavorable decision.
Appeal rights include:
- Right to request a fair hearing.
- Opportunity to present evidence and arguments.
- Notification of denial reasons and appeal instructions.
4. How Partnerships Can Influence Medicaid Eligibility
Strategic partnerships can offer financial stability and potentially affect Medicaid eligibility.
Partnerships can play a significant role in influencing Medicaid eligibility by providing financial stability and income opportunities. Collaborating with others can lead to increased income, which may affect your eligibility for Medicaid. Understanding how these partnerships can impact your financial situation is crucial for managing your healthcare coverage.
4.1 What Types of Partnerships Can Impact My Income?
Various partnerships, from business ventures to joint projects, can impact your income and Medicaid eligibility.
Several types of partnerships can influence your income, including business partnerships, joint ventures, and freelance collaborations. Business partnerships involve pooling resources and expertise to start or grow a business, potentially leading to increased profits. Joint ventures involve collaborating on specific projects or ventures, sharing both the risks and rewards. Freelance collaborations involve working with others on a project basis, providing opportunities to earn additional income. Each type of partnership offers unique benefits and can impact your financial situation differently.
Types of partnerships:
- Business partnerships.
- Joint ventures.
- Freelance collaborations.
4.2 How Can I Structure Partnerships to Maintain Medicaid Eligibility?
Careful planning can help structure partnerships to balance income and maintain Medicaid eligibility.
Structuring partnerships to maintain Medicaid eligibility requires careful planning and consideration of income limits. One strategy is to ensure that partnership income is structured in a way that doesn’t exceed the Medicaid income threshold. This may involve setting up the partnership to distribute income in specific intervals or reinvesting profits back into the business to reduce taxable income. Consulting with a financial advisor can provide personalized guidance on structuring partnerships to optimize income and maintain Medicaid eligibility.
Strategies for structuring partnerships:
- Distribute income strategically.
- Reinvest profits to reduce taxable income.
- Consult with a financial advisor.
4.3 What Resources Are Available to Help Me Find Suitable Partners?
Websites like income-partners.net can help you connect with potential partners and explore income-generating opportunities.
Finding suitable partners can be facilitated by leveraging online platforms and networking events. Websites like income-partners.net specialize in connecting individuals with potential partners and opportunities for collaboration. Networking events, industry conferences, and business associations also provide valuable avenues for meeting like-minded individuals and exploring partnership opportunities. Utilizing these resources can increase your chances of finding partners that align with your goals and can contribute to your financial well-being.
Resources for finding partners:
- Online platforms like income-partners.net.
- Networking events and industry conferences.
- Business associations.
4.4 How Does income-partners.net Support Partnership Opportunities?
Income-partners.net offers a platform to explore various partnership models and strategies for increased income.
Income-partners.net is designed to support partnership opportunities by providing a platform for individuals to connect, collaborate, and explore income-generating ventures. The website offers resources and tools to help you identify potential partners, evaluate partnership models, and develop strategies for increasing your income. By leveraging income-partners.net, you can access a network of like-minded individuals and explore diverse opportunities to improve your financial stability.
Income-partners.net offers:
- A platform for connecting with potential partners.
- Resources to evaluate partnership models.
- Strategies for increasing income.
5. Medicaid and Self-Employment Income: Key Considerations
Self-employment income requires careful management to maintain Medicaid eligibility.
Self-employment income requires careful management to ensure continued Medicaid eligibility. Unlike traditional employment, self-employment income can fluctuate, making it challenging to predict and manage. Understanding how Medicaid assesses self-employment income and implementing strategies to manage it effectively is crucial for maintaining your healthcare coverage.
5.1 How Does Medicaid Calculate Self-Employment Income?
Medicaid assesses self-employment income by considering business expenses and net earnings.
Medicaid calculates self-employment income by considering both your gross income and allowable business expenses. Net self-employment income, which is your gross income minus business expenses, is the figure used to determine Medicaid eligibility. It’s essential to keep accurate records of all income and expenses to ensure an accurate assessment. Additionally, some states may have specific rules or deductions that can further impact your countable income.
Calculation process:
- Gross income minus allowable business expenses.
- Net self-employment income determines eligibility.
- Accurate record-keeping is essential.
5.2 What Business Expenses Can Be Deducted From My Income?
Understanding deductible business expenses can help lower your countable income for Medicaid.
Various business expenses can be deducted from your self-employment income, reducing your countable income for Medicaid purposes. Common deductible expenses include costs for supplies, equipment, advertising, rent, utilities, and transportation. Keeping detailed records of these expenses is crucial for substantiating your deductions. Consult with a tax professional to ensure you’re claiming all eligible deductions.
Common deductible expenses:
- Supplies and equipment.
- Advertising and marketing costs.
- Rent and utilities.
- Transportation expenses.
5.3 How Can I Plan for Fluctuating Self-Employment Income?
Strategies like budgeting and savings can help manage income fluctuations and maintain Medicaid eligibility.
Planning for fluctuating self-employment income involves implementing strategies to manage income variations and maintain Medicaid eligibility. Budgeting, setting aside savings during high-income periods, and exploring strategies to stabilize income can help you navigate these fluctuations. Additionally, understanding the Medicaid reporting requirements for self-employment income is essential for staying compliant and avoiding eligibility issues.
Strategies for managing fluctuations:
- Budgeting and savings.
- Stabilizing income through diversified projects.
- Understanding Medicaid reporting requirements.
5.4 When Should I Report Changes in My Self-Employment Income to Medicaid?
Timely reporting of income changes is essential to maintain Medicaid eligibility and avoid complications.
Reporting changes in your self-employment income to Medicaid is crucial for maintaining accurate eligibility status. Most states require you to report income changes promptly, typically within 10 to 30 days of the change. Failure to report changes can lead to inaccuracies in your eligibility determination and potential penalties. Staying proactive in reporting income changes can help you avoid complications and maintain uninterrupted Medicaid coverage.
Reporting guidelines:
- Report income changes promptly.
- Typically within 10 to 30 days of the change.
- Avoid penalties by staying proactive.
6. Additional Resources and Support for Medicaid Applicants
Numerous resources are available to support you through the Medicaid application process.
Navigating the Medicaid system can be challenging, but numerous resources are available to provide support and guidance. From government agencies to non-profit organizations, these resources can help you understand eligibility requirements, complete the application process, and access the benefits you’re entitled to.
6.1 Where Can I Find State-Specific Medicaid Information?
Each state’s Medicaid website offers detailed information on eligibility, benefits, and application procedures.
Finding state-specific Medicaid information is essential for understanding the unique requirements and benefits in your location. Each state operates its own Medicaid program, and the eligibility criteria, covered services, and application procedures can vary. Visiting your state’s Medicaid website is the best way to access accurate and up-to-date information. These websites provide detailed guides, contact information, and online application portals.
Sources for state-specific information:
- State Medicaid websites.
- Local Medicaid offices.
- State health departments.
6.2 Are There Nonprofit Organizations That Can Assist With Medicaid Enrollment?
Nonprofit organizations often provide free assistance with Medicaid enrollment and navigation.
Nonprofit organizations play a vital role in assisting individuals with Medicaid enrollment and navigation. These organizations often provide free services, such as application assistance, eligibility screening, and information about available benefits. They can help you understand the complexities of the Medicaid system and ensure you receive the support you need to access healthcare coverage.
Examples of nonprofit support:
- Application assistance.
- Eligibility screening.
- Information about available benefits.
6.3 What Is the Role of Healthcare Navigators in the Medicaid Process?
Healthcare navigators offer personalized assistance to help individuals understand and enroll in Medicaid.
Healthcare navigators are trained professionals who provide personalized assistance to individuals seeking to understand and enroll in Medicaid. They can help you navigate the application process, understand eligibility requirements, and explore available healthcare options. Navigators offer unbiased information and support, ensuring you make informed decisions about your healthcare coverage.
Navigator services include:
- Application assistance.
- Eligibility guidance.
- Healthcare options counseling.
6.4 How Can I Stay Updated on Changes to Medicaid Policies?
Staying informed about Medicaid policy changes ensures you remain compliant and eligible.
Staying updated on changes to Medicaid policies is crucial for ensuring you remain compliant and eligible for benefits. Medicaid policies can change due to legislative updates, regulatory changes, or state-specific initiatives. Subscribing to newsletters, following relevant government websites, and consulting with healthcare professionals can help you stay informed about these changes.
Methods for staying informed:
- Subscribing to newsletters.
- Following government websites.
- Consulting with healthcare professionals.
7. Maximizing Income and Maintaining Medicaid: A Balanced Approach
Balancing income growth with Medicaid eligibility requires strategic financial planning.
Maximizing income while maintaining Medicaid eligibility requires a balanced approach that combines financial planning with an understanding of Medicaid rules. Strategies such as structuring partnerships effectively, managing self-employment income, and leveraging available resources can help you achieve both financial stability and access to healthcare coverage.
7.1 How Can I Create a Financial Plan That Considers Medicaid Eligibility?
A comprehensive financial plan should integrate strategies to manage income and maintain Medicaid eligibility.
Creating a financial plan that considers Medicaid eligibility involves integrating strategies to manage income, expenses, and assets in a way that aligns with Medicaid requirements. This may include setting income goals that remain within Medicaid limits, exploring options for reinvesting income to reduce taxable income, and consulting with a financial advisor to develop a personalized plan. A well-crafted financial plan can help you achieve your financial goals while maintaining access to essential healthcare services.
Key components of a financial plan:
- Setting income goals within Medicaid limits.
- Reinvesting income to reduce taxable income.
- Consulting with a financial advisor.
7.2 What Are the Long-Term Benefits of Strategic Partnerships?
Strategic partnerships can provide sustained income growth and stability, impacting long-term Medicaid eligibility.
Strategic partnerships offer numerous long-term benefits, including sustained income growth, increased financial stability, and access to new opportunities. By collaborating with others, you can leverage diverse skills and resources to achieve greater success. This can lead to increased income, which may impact your Medicaid eligibility over time. However, with careful planning, you can structure partnerships to optimize income while maintaining access to healthcare coverage.
Long-term partnership benefits:
- Sustained income growth.
- Increased financial stability.
- Access to new opportunities.
7.3 How Does income-partners.net Help Me Achieve Financial Stability?
Income-partners.net provides tools and resources to build successful partnerships and enhance financial well-being.
Income-partners.net is designed to help you achieve financial stability by providing tools and resources to build successful partnerships. The website offers a platform for connecting with potential partners, evaluating partnership models, and developing strategies for increasing your income. By leveraging income-partners.net, you can access a network of like-minded individuals and explore diverse opportunities to improve your financial well-being.
Income-partners.net features:
- Platform for connecting with partners.
- Resources to evaluate partnership models.
- Strategies for increasing income.
7.4 What Steps Should I Take to Start Building Strategic Partnerships Today?
Starting with clear goals and utilizing online platforms like income-partners.net can kickstart your partnership journey.
To start building strategic partnerships today, begin by identifying your goals, skills, and what you seek in a partner. Utilize online platforms like income-partners.net to connect with potential collaborators. Attend networking events and industry conferences to meet like-minded individuals. By taking these steps, you can kickstart your partnership journey and unlock opportunities for financial growth and stability.
Initial steps:
- Identify your goals and skills.
- Utilize online platforms.
- Attend networking events.
FAQ: Understanding Medicaid and Income
1. Is Medicaid strictly based on income?
Yes, Medicaid eligibility is primarily income-based, but other factors like age, disability, and residency also play a role.
2. How does MAGI affect Medicaid eligibility?
MAGI (Modified Adjusted Gross Income) is the standard method for determining income eligibility for most Medicaid applicants, considering taxable income and tax filing relationships.
3. What happens if my income exceeds the Medicaid limit?
You may still qualify through options like the Medically Needy program or a spend-down program, which allow you to deduct medical expenses from your income.
4. Are there different Medicaid rules for children and pregnant women?
Yes, children and pregnant women often have more lenient income requirements for Medicaid eligibility, with higher income thresholds and specific coverage for prenatal care.
5. How can partnerships impact my Medicaid eligibility?
Partnerships can increase your income, potentially affecting Medicaid eligibility. Careful planning is needed to structure partnerships in a way that balances income growth and maintains eligibility.
6. How does Medicaid calculate self-employment income?
Medicaid calculates self-employment income by considering your gross income minus allowable business expenses to determine your net self-employment income.
7. What business expenses can be deducted from my self-employment income?
Common deductible expenses include costs for supplies, equipment, advertising, rent, utilities, and transportation. Keeping detailed records is crucial.
8. Where can I find state-specific Medicaid information?
Each state’s Medicaid website offers detailed information on eligibility, benefits, and application procedures specific to that state.
9. Can nonprofit organizations assist with Medicaid enrollment?
Yes, many nonprofit organizations provide free assistance with Medicaid enrollment, including application help and eligibility screening.
10. How can income-partners.net help me achieve financial stability while considering Medicaid?
Income-partners.net offers a platform to explore various partnership models and strategies for increased income, helping you achieve financial stability while considering Medicaid eligibility.
Medicaid eligibility hinges significantly on income, but understanding the nuances and available strategies can help you navigate the system effectively. Whether you’re exploring partnership opportunities or managing self-employment income, resources like income-partners.net can provide valuable support.
Explore partnership opportunities, learn effective relationship-building strategies, and connect with potential partners in the U.S. on income-partners.net today. Address: 1 University Station, Austin, TX 78712, United States. Phone: +1 (512) 471-3434.